Caregiver burnout is an epidemic. At the end of 2021, nearly 63% of physicians reported symptoms of burnout, up from 38% in 2020[1]. What’s causing these unprecedented levels of caregiver dissatisfaction? Often, it’s the ‘hassle factors’ that cause burnout - system inefficiencies, administrative burdens and increased regulation and technology requirements (such as EHRs)[2].
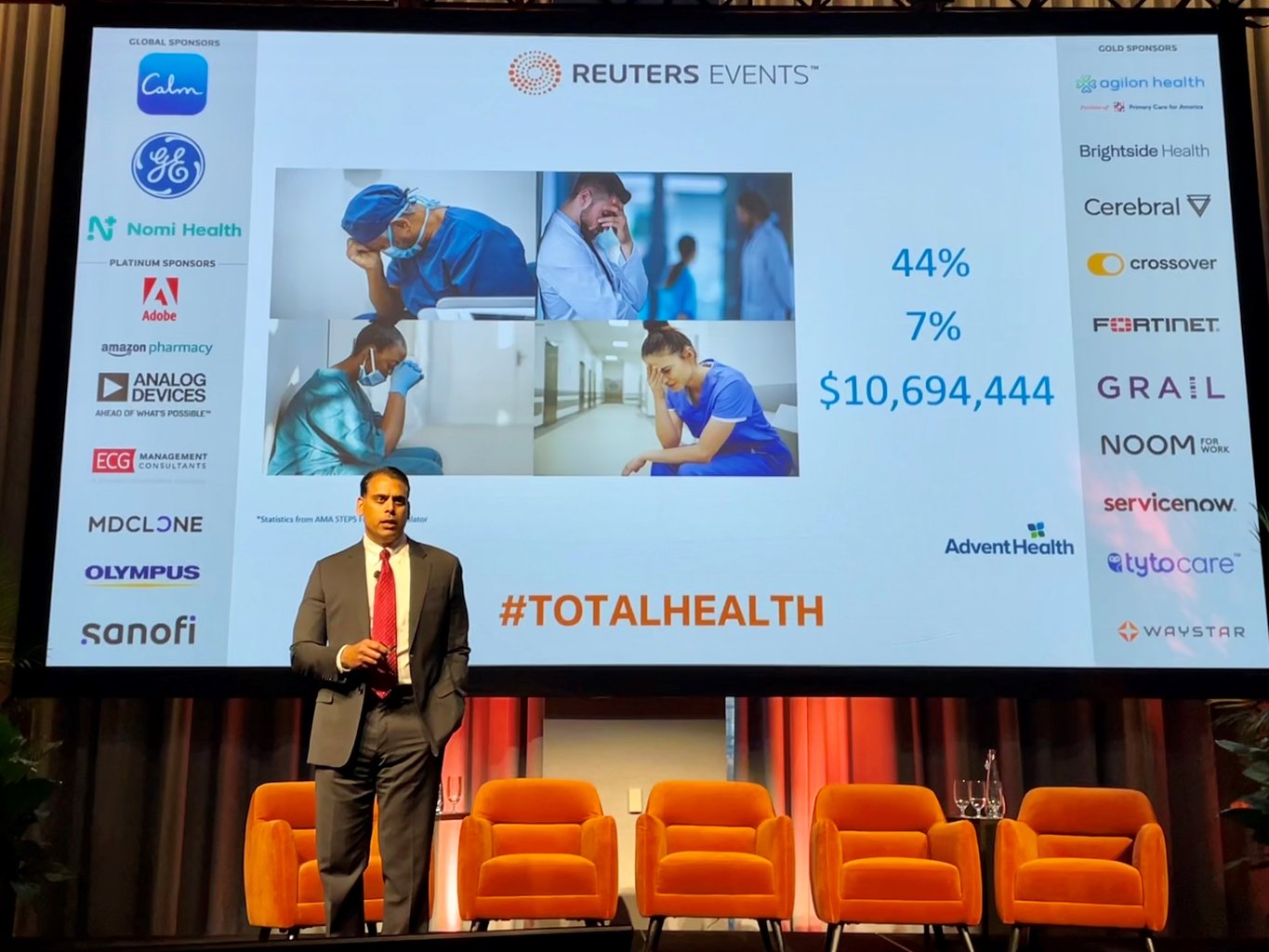
At the Reuters Total Health event, Dr. Sanjay Pattani, Associate Chief Medical Officer of Mission Control at AdventHealth in Central Florida provided strategies to address burnout. Here are some of the insights he shared during the session “Combat stress, fatigue and burnout within your organization.”
Many industries have realized widespread success using digital process automation to streamline repetitive processes and reduce manual tasks. While healthcare has seen some success with automating medical billing and coding, using automation to streamline clinical care at the bedside has been less successful.
An electronic health record helps facilitate the exchange of information as patients move from venue to venue, but the arduous task of entering that information often causes an overall lack of efficiency. Health system leaders need to ask, “Are we working harder and not smarter?”
AdventHealth in Central Florida is committed to executing more intentionally. Their technology initiatives link process and workflow improvement to their data automation strategies. A focus on making processes easier for patients and the providers taking care of those patients led to a partnership with GE HealthCare’s Command Centers team to launch their Mission Control Command Center.
Complementing their electronic health record, Mission Control provides real time situational awareness. It also simplifies communication amongst more than 6500 team members across nine hospitals.
The Command Center uses AI and predictive analytics to centrally manage capacity across the entire system. Equally important is the impact at the patient level. The digital platform provides actionable insights that intelligently assist providers in the delivery of care. Here are some examples Dr. Pattani provided:
- Well-coordinated patient discharges – With Tiles (apps) that focus on care progression and care transition, everyone who cares for the patient is informed and in sync. Each member of the care team can align their workflows to expedite patient care – including the complex discharge process.
- Faster, easier and smarter rounding huddles – The Command Center technology helps coordinate exactly what needs to get done and who is accountable for each task. That speeds up the exchange of information and decision-making. As a result, speed rounds have gone from 2-3 minutes per patient to just 30 seconds.
- Prioritization of patient placements – The time from bed request to assignment was shaved by over 45 minutes. That equates to saving over 50 excess days per year.
- Strategic capacity management – Senior leadership can see exactly which resources are in high demand and where the demand is most acute. That enables them to pull the necessary levers to organize supply around demand.
These efficiencies benefit both patients and providers, giving caregivers more time to spend at the bedside. Fewer phone calls, streamlined workflows and better collaboration improve care delivery to help alleviate the stress, fatigue, and burnout.
As we seek to improve care delivery for patients, we must also make intentional commitments to the well-being of the workforce. The digitization of healthcare is ultimately a humanistic practice. The data points are all patients. Caring for those patients is a team of humans. We cannot lose sight of how that care is provided and how we protect the caregivers.
[1]American Medical Association, https://www.ama-assn.org/practice-management/physician-health/measuring-and-addressing-physician-burnout
[2]American Medical Association, https://www.ama-assn.org/practice-management/physician-health/what-physician-burnout